Health Net 2015 Annual Report Download - page 16
Download and view the complete annual report
Please find page 16 of the 2015 Health Net annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.14
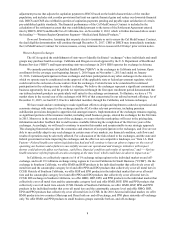
generally compete for state Medicaid contracts with other managed health care companies, both for profit and not-for-
profit.
Our Oregon health plan competes primarily with Cambia Health Solutions, Kaiser Permanente, Providence
Health Plan, Moda Health Plan, Inc., and PacificSource Health.
With respect to the our TRICARE, MFLC and PC3 contracts, our primary competitors in the bidding process
include Humana, United HealthGroup, Inc., Aetna, Inc., Anthem, Inc., Magellan Health Services, Beacon Health
Options, Inc. and TriWest Healthcare Alliance, among others.
If we fail to compete effectively to maintain or increase our market share, our results of operations, financial
condition and cash flows could be materially adversely affected. For additional information on competitive conditions
in our business, see “Item 1A. Risk Factors—The markets in which we do business are highly competitive. If we do not
design and price our product offerings competitively, our membership and profitability could decline.”
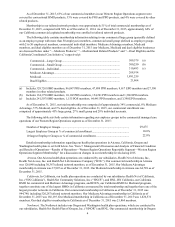
Cognizant Transaction
On November 2, 2014, we entered into a Master Services Agreement (as subsequently amended and restated, the
"Master Services Agreement") with Cognizant Healthcare Services, LLC, a wholly owned subsidiary of Cognizant
Technology Solutions Corporation (collectively, "Cognizant"). Under the terms of the Master Services Agreement,
Cognizant agreed to, among other things, provide us with certain consulting, technology and administrative services in
the following areas: claims management, membership and benefits configuration, customer contact center services,
information technology, quality assurance, appeals and grievance services, and non-clinical medical management
support (collectively, the "BP and IT Services"). Concurrent with executing the Master Services Agreement, we entered
into the Asset Purchase Agreement with Cognizant, through which Cognizant agreed to purchase certain software assets
and related intellectual property from us for $50 million (the "Asset Sale"). See Note 3 to our consolidated financial
statements for additional information. However, in connection with the announcement of the Merger with Centene, the
parties agreed to suspend efforts towards, and defer the occurrence of, the BPaaS Services Commencement Date (as
defined in the Master Services Agreement). Accordingly, on July 1, 2015, the parties entered into an amendment to the
Master Services Agreement (the “Cognizant Amendment”) which, among other things, extended the Pre-BPaaS
Services Commencement Date Termination period, or the period of time during which the Company may terminate the
Cognizant Agreement for a break-up fee of $10 million, until after the closing of the Merger. Cognizant continues to
provide certain application and business processing services pursuant to existing agreements it has with us. The
Company and Cognizant have agreed to exercise good faith efforts to explore and, if both parties agree to proceed, to
negotiate and enter into a new definitive agreement relating to certain services described in the Master Services
Agreement, which new definitive agreement shall survive the closing of the Merger.
The closing of the Asset Sale was scheduled for the BPaaS Services Commencement Date. As a result, the
parties’ aforementioned decision to suspend efforts towards the BPaaS Services Commencement Date has similarly
deferred the Asset Sale.
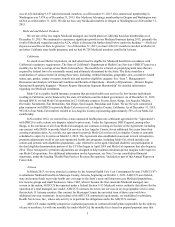
Marketing and Sales
We market our products and services to individuals and employer groups through internal sales staff, independent
brokers, agents and consultants and through the Internet and the ACA exchanges. For our group health business, we
market our products and services utilizing a three-step process. We first market to potential employer groups, group
insurance brokers and consultants. We then provide information directly to employees once the employer has selected
our health coverage. Finally, we engage members and employers in marketing for member and group retention. For our
large group business, in general, we solicit enrollees from the employee base directly during “open enrollment” periods
when employees are permitted to change health care programs. We use a variety of techniques to attract new enrollees
and retain existing members, which at times include, without limitation, direct mail, work day and health fair
presentations and telemarketing. Similar methods are used by our Medicare business to market to eligible individuals.
Our sales efforts are supported by our marketing division, which engages in product research and development,
multicultural marketing, advertising and communications, and member education and retention programs. The
establishment of the exchanges under the ACA created a new competitive insurance marketplace for individuals and
small businesses. As these exchanges mature, we have refined and enhanced our exchange related marketing strategies,
particularly to individuals.
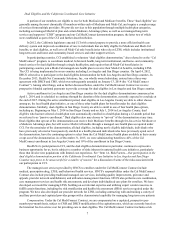
Premiums for each employer group are generally contracted on a yearly basis and are payable monthly. We
consider numerous factors in setting our monthly premiums, including changes in benefit design to address employer
group needs and anticipated health care utilization rates as forecast by us based on the demographic composition of, and
our prior experience in, our service areas. Premiums are also affected by applicable state and federal law and