Quest Diagnostics 1996 Annual Report Download - page 12
Download and view the complete annual report
Please find page 12 of the 1996 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
11
grams and underlying systems that
will enable us to pay our sales organi-
zation based on profitability, and have
pilot programs in certain locations
this year.
Turning Data Into Information
The massive amounts of data generat-
ed by our testing processes represent
a valuable database resource for
health care companies. Our two year
old venture called Quest Informatics
turns our testing data into informa-
tion and supplies it to large health
care buyers that use this knowledge
to help them better manage their
patients’ disease states.
One managed care company on the
East Coast uses this information to
help it monitor and manage diabetic
members who are employees of a sin-
gle member company. Specifically,
the managed care company requires
test results every time one of their
diabetic patients has a test performed
at one of our labs. Searching through
millions of records for a few hundred
test results is an information technol-
ogy challenge of the highest order.
Quest Informatics designed a screen-
ing process and an electronic bridge
connecting our mainframe comput-
ers to the managed care client.
Whenever a diabetic employee is test-
ed and the result is within a specified
range, the results are transmitted
electronically to a disease manager
who specializes in diabetes. Now, the
managed care company can target its
resources for educating patients on
diabetes to the individuals who need
it most and then closely monitor their
ed to provide, we are selectively rene-
gotiating our relationships. In New
England, for example, we were asked
by a large managed care organization
to provide services under a national
contract that was priced below our
cost. Because physicians in the region
are familiar with our high level of ser-
vice and quality, we were able to suc-
cessfully renegotiate the contract away
from a capitated rate, or one in which
we were paid a fixed monthly fee per
member of the plan, to a fee-for-ser-
vice arrangement at a rate that
ensured the contract would be both
profitable to us and valuable to our
customer.
On the West Coast, we approached a
major third party payor about raising
its reimbursement levels for the Pap
smear, a labor-intensive cervical cancer
screen for women that is performed
by highly trained cytotechnologists.
Our people went back to the third
party payor and presented our num-
bers, which showed we were being
paid for Pap smears at a rate well
below our cost. Based on our analysis,
the payor acknowledged the fairness
of our position and more than
doubled the reimbursement rate on
Pap smears.
Part of the problem we have had with
pricing is that our employees’ interests
haven’t always been aligned with the
company’s long-term interests.
Compensation for our sales represen-
tatives was based solely on new sales
volume, not profitability. That’s now
changing. We are designing the pro-
progress. Research shows that rigor-
ous monitoring of diabetes patients
can prevent complications later on
and save money for the managed care
provider. Quest Informatics receives a
transaction fee each time a result is
sent over its electronic bridge.
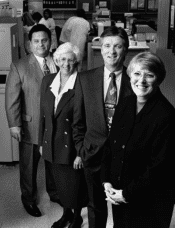
We recently expanded our
decade-long laboratory
partnership with the two
leading hospitals in Erie, Pa.,
to cover an additional 17
hospitals in the region. Here,
Sister Catherine Manning,
President of Saint Vincent
Health Center (second from
left) and John Malone,
President of Hamot
Health Foundation
(second from right), meet with
Tony Geramita of
Quest Diagnostics and
Karen Case of Associated
Clinical Laboratories.