Health Net 2014 Annual Report Download - page 6
Download and view the complete annual report
Please find page 6 of the 2014 Health Net annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.4
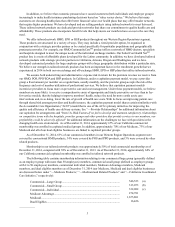
(a) Includes 360,901 HMO members, 92,849 POS members, 58,802 PPO members, 9,461 EPO members and 24,510
members in other related products.
(b) Includes 153,299 HMO members, 21,021 POS members, 137,717 PPO members and 1,036 EPO members.
(c) Includes 233,696 HMO members, 2,842 POS members, 95,521 PPO members, and 23 EPO members.
As of December 31, 2014, our total membership was comprised of approximately 38% commercial, 8% Medicare
Advantage, 53% Medicaid, and 1% dual eligibles. As of December 31, 2014, our commercial enrollment was
comprised of approximately 46% large group, 26% small group and 28% individual accounts. Our membership in
individual accounts increased from 11% of our commercial enrollment as of December 31, 2013, driven in large part by
membership increases in the health insurance exchanges, which are further described below under the heading “—
Western Region Exchanges.”
The following table sets forth certain information regarding our employer groups in the commercial managed care
operations of our Western Region Operations segment as of December 31, 2014:
Number of Employer Groups................................................................................................ 27,965
Largest Employer Group as % of commercial enrollment.................................................... 9.0%
10 largest Employer Groups as % of commercial enrollment............................................... 21.4%
Detailed membership information regarding our health plan operations in Arizona, California, Oregon and
Washington health plans is set forth below. See “Item 7. Management's Discussion and Analysis of Financial Condition
and Results of Operations—Results of Operations—Western Region Operations Reportable Segment—Western Region
Operations Segment Membership” for a discussion on changes in our membership levels during 2014.
Arizona. Our Arizona health plan operations are conducted by our subsidiaries, Health Net of Arizona, Inc.,
Health Net Access, Inc. and Health Net Life Insurance Company (“HNL”). Our commercial membership in Arizona
was 178,064 including 60,743 tailored network members, as of December 31, 2014. Our Medicare Advantage
membership in Arizona was 45,873 as of December 31, 2014. Our Medicaid membership in Arizona was 80,913 as of
December 31, 2014.
California. In California, our health plan operations are conducted by our subsidiaries Health Net of California,
Inc. (“HN California”), Health Net Community Solutions, Inc. (“HNCS”), and HNL. HN California, our California
HMO for commercial and Medicare Advantage programs, and HNCS, our California HMO for Medicaid programs,
together constitute one of the largest HMOs in California as measured by total membership and together have one of the
largest provider networks in California. Our commercial membership in California as of December 31, 2014 was
957,495, including 523,890 tailored network members. Our Medicare Advantage membership in California as of
December 31, 2014 was 172,554. Our Medicaid membership in California as of December 31, 2014 was 1,594,888
members. Our dual eligibles membership in California as of December 31, 2014 was 16,426 members.
Northwest. The Northwest includes our Oregon and Washington health plan operations, which are conducted by
our subsidiaries, Health Net Health Plan of Oregon, Inc. (“HNOR”) and HNL. Our commercial membership in Oregon
was 47,646 including 8,240 tailored network members, as of December 31, 2014. Our commercial membership in
Washington was 8,473 as of December 31, 2014. Our Medicare Advantage membership in Oregon and Washington was
56,354 as of December 31, 2014. We did not have any Medicaid members in Oregon or Washington as of December 31,
2014.
Medicaid and Related Products
We are one of the two largest Medicaid managed care health plans in California based on membership as of
December 31, 2014. We experienced significant growth in our Medicaid business during 2014, primarily the result of
Medicaid expansion under the ACA, which is discussed in further detail below under the heading “—Medicaid
Expansion and Recent State Legislation.” As of December 31, 2014, we had 1,594,888 members enrolled in Medi-Cal
and other California state health programs, and we had 80,913 Medicaid members enrolled in Arizona.
California
To enroll in our Medi-Cal products, an individual must be eligible for Medicaid benefits in accordance with
California's regulatory requirements. The State of California's Department of Health Care Services (“DHCS”) pays us a
monthly fee for the coverage of our Medicaid members. The monthly fee is based on prepaid payment rates that are
required by federal law to be actuarially sound, and ultimately determined by the State. The State considers a
combination of various factors in setting these rates, including, without limitation, geographic area, a member's health