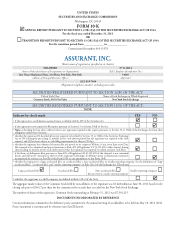
Assurant 2011 Annual Report Download - page 19
Download and view the complete annual report
Please find page 19 of the 2011 Assurant annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.ASSURANT, INC.2011 Form10-K 11
PARTI
ITEM 1 Business
Dividend Payment Limitations
e Company’s assets consist primarily of the capital stock of our
subsidiaries. Accordingly, our future cash ows depend upon the availability
of dividends and other statutorily permissible payments from our
subsidiaries. e ability to pay such dividends and to make such other
payments is regulated by the states in which our subsidiaries are domiciled.
ese dividend regulations vary from state to state and by type of insurance
provided by the applicable subsidiary, but generally require our insurance
subsidiaries to maintain minimum solvency requirements and limit the
amount of dividends these subsidiaries can pay to the holding company.
For more information, please see Item7, “Management’s Discussion and
Analysis of Financial Condition and Results of Operations—Liquidity
and Capital Resources—Regulatory Requirements.”
Risk Based Capital Requirements
In order to enhance the regulation of insurer solvency, the National
Association of Insurance Commissioners (“NAIC”) has established certain
risk-based capital standards applicable to life, health and property and
casualty insurers. Risk-based capital, which regulators use to assess the
su ciency of an insurer’s statutory capital, is calculated by applying
factors to various asset, premium, expense, liability and reserve items.
Factors are higher for items which in the NAIC’s view have greater
underlying risk. e NAIC periodically reviews the risk-based capital
formula and changes to the formula could occur in the future.
Investment Regulation
Insurance company investments must comply with applicable laws
and regulations that prescribe the kind, quality and concentration
of investments. ese regulations require diversi cation of insurance
company investment portfolios and limit the amount of investments
in certain asset categories.
Financial Reporting
Regulators closely monitor the nancial condition of licensed insurance
companies and our insurance subsidiaries are required to le periodic
nancial reports with insurance regulators. Moreover, states regulate
the form and content of these statutory nancial statements.
Products and Coverage
Insurance regulators have broad authority to regulate many aspects
of our products and services. For example, some jurisdictions require
insurers to provide coverage to persons who would not be considered
eligible insurance risks under standard underwriting criteria, dictating
the types of insurance and the level of coverage that must be provided
to such applicants. Additionally, certain non-insurance products and
services, such as service contracts, may be regulated by regulatory bodies
other than departments of insurance.
Pricing and Premium Rates
Nearly all states have insurance laws requiring insurers to le price
schedules and policy forms with the state’s regulatory authority. In many
cases, these price schedules and/or policy forms must be approved prior
to use, and state insurance departments have the power to disapprove
increases or require decreases in the premium rates we charge.
Market Conduct Regulation
Activities of insurers are highly regulated by state insurance laws
and regulations, which govern the form and content of disclosure to
consumers, advertising, sales practices and complaint handling. State
regulatory authorities enforce compliance through periodic market
conduct examinations.
Guaranty Associations and Indemnity Funds
Most states require insurance companies to support guaranty associations
or indemnity funds, which are established to pay claims on behalf of
insolvent insurance companies. ese associations may levy assessments
on member insurers. In some states member insurers can recover
a portion of these assessments through premium tax o sets and/or
policyholder surcharges.
Insurance Regulatory Initiatives
e NAIC, state regulators and professional organizations have
considered and are considering various proposals that may alter or
increase state authority to regulate insurance companies and insurance
holding companies. Please see Item1A, “Risk Factors—Risks Related
to Our Industry—Changes in regulation may reduce our pro tability
and limit our growth” for a discussion of the risks related to such
initiatives.
Federal Regulation
Patient Protection and Aff ordable Care Act
Although health insurance is generally regulated at the state level,
recent legislative actions were taken at the federal level that impose
added restrictions on our business, in particular Assurant Health and
Assurant Employee Bene ts. In March2010, President Obama signed
the A ordable Care Act into law. Provisions of the A ordable Care
Act and related reforms have and will continue to become e ective at
various dates over the next several years. ese provisions and related
impacts include a requirement that we pay rebates to customers if
the loss ratios for some of our products lines are less than speci ed
percentages; the reduction of agent commissions, and the consequent
risk that insurance producers may sell less of our products than they
have in the past; changes in the bene ts provided under some of our
products; elimination of limits on lifetime and annual bene t maximums;
a prohibition from imposing any pre-existing condition exclusion as it
applies to enrollees under the age of 19 who apply for coverage; limits
on our ability to rescind coverage for persons who have misrepresented
or omitted material information when they applied for coverage and,
after January1,2014, elimination of our ability to underwrite health
insurance products with certain narrow exceptions; a requirement to
o er coverage to any person who applies for such coverage; increased
costs to modify and/or sell our products; intensi ed competitive
pressures that limit our ability to increase rates due to state insurance
exchanges; signi cant risk of customer loss; new and higher taxes and
fees; and the need to operate with a lower expense structure at both
the business segment and enterprise level.