Health Net 2004 Annual Report Download - page 10
Download and view the complete annual report
Please find page 10 of the 2004 Health Net annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
regions) and September 1, 2004 for the area that was previously TRICARE Region 1 (now referred to as the National Capital and
Northeast sub-regions).
Health care delivery ended under our former Region 11 contract on May 31, 2004, our former Regions 9, 10 and 12 contract on
June 30, 2004, and our former Region 6 contract on October 31, 2004.
Eligible beneficiaries in the TRICARE program are able to choose from a variety of program options. They can choose to enroll
in TRICARE Prime, which is similar to a conventional HMO plan, or they can select, on a case-by-case basis, to utilize TRICARE
Extra, which is similar to a conventional PPO plan, or TRICARE Standard, which is similar to a conventional indemnity plan.
Under TRICARE Prime, enrollees pay an enrollment fee (which is zero for active duty participants and their dependents) and
select a primary care physician from a designated provider panel. The primary care physicians are responsible for making referrals to
specialists and hospitals. Except for active duty family members who have no co-payment charges, TRICARE Prime enrollees pay
co-payments each time they receive medical services from a civilian provider. TRICARE Prime enrollees may opt, on a case-by-case
basis, for a point-of-service option in which they are allowed to self-refer but incur a deductible and a co-payment.
Under TRICARE Extra, eligible beneficiaries may utilize a TRICARE network provider but incur a deductible and co-payment
which is greater than the TRICARE Prime co-payment. Under TRICARE Standard, eligible beneficiaries may utilize a TRICARE
authorized provider who is not a network provider but pay a higher co-payment than under TRICARE Prime or TRICARE Extra.
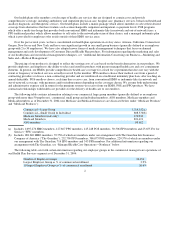
As of December 31, 2004, there were 1,350,153 TRICARE eligibles enrolled in TRICARE Prime under our North Region
contract. The total estimated number of eligible beneficiaries for the North Region contract as of December 31, 2004, based on data
provided by the Department of Defense, was 2,928,627.
There are certain differences in the economic structure of the new TRICARE contract for the North Region as compared to our
old TRICARE contracts. The old TRICARE contracts included a fixed price for health care costs for the term of the contracts, subject
to adjustment based primarily on the number of TRICARE eligibles and utilization of services within military hospitals and clinics,
with underruns and overruns of our fixed price provision borne 70% by the government and 30% by us. The new TRICARE contract
includes a target price for the cost reimbursed health care costs which is negotiated annually during the term of the contract, with
underruns and overruns of our target price provision borne 80% by the government and 20% by us. Under our old contracts, the
administrative price was fixed, whereas under the new contract certain components of the administrative price are subject to volume-
based adjustments.
With respect to cash flow, under the old contracts we were paid monthly based on incurred claims with an annual reconciliation
of the risk sharing provision. Under the new contract, we are paid within five days for each claims run based on paid claims with an
annual reconciliation of the risk sharing provision. Under the old contracts, we were responsible for providing pharmaceutical
benefits, claims processing for TRICARE and Medicare dual eligibles and certain marketing and education services that we will not
provide under the new contract. Under the old contracts and the new contract, the administrative price is paid on a monthly basis, one
month in arrears.
We believe that the changes in the economic structure of the new TRICARE contract, when compared to our old TRICARE
contracts, should reduce our risk related to the ability to accurately project our profitability over the term of the new contract. For
additional information regarding our TRICARE contract for the North Region, see “Item 7. Management’s Discussion and Analysis
of Financial Condition and Results of Operations.”
7